Oliver Sacks, who has taught us so much, now teaches us the art of dying
Death is never easy. But Oliver Sacks shows us an approach that views life as a welcome gift rather than bemoaning death as a medical failure
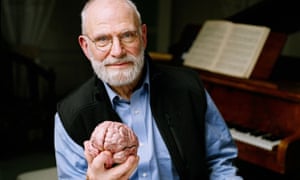
Like millions of readers I had a lump in my throat as I read Oliver Sacks reveal his diagnosis of terminal cancer earlier this year. Every doctor aspires to be a little like Sacks whether for his sharp intellect, his obvious humanity or his exquisite writings that go to the core of what it means to be human and frail.
In February he calmly declared that metastatic melanoma affecting his liver meant that his luck had run out. I found it hard to share his calm but then like the genial, grandfather-figure he is, he reassured us, oncologists and all, that he still felt intensely alive, wanting to “deepen my friendships, to write more, to achieve new levels of understanding and insight.”
His mention of finding a new focus and perspective resonated with me – it is as close to a universal finding as there is in clinic, where ordinary individuals and famous people all say that cancer forced them to contemplate their life and legacy.
It’s not always pretty, I concede. Cancer triggers joyful marriage but also bitter divorce. It unites bickering siblings but also tears apart those previously contented. It fosters a peaceful reckoning and loving coexistence but equally tempestuous anger and unrelenting sorrow. All I can say is letting go is hard. Actually, it sucks. Watching the march of thousands of such patients, I keep thinking it must be indescribably difficult to bear if it is so difficult just to watch from the vantage point of an unrelated oncologist, who at best catches only glimpses of the struggle patients face every day.
The lump in my throat grew larger this weekend when Oliver Sacks declared that his disease had inevitably returned despite liver embolization and immunotherapy, the holy grail of melanoma treatment. Oh no, I thought glumly, not you too, as if the greatness of being Oliver Sacks were enough to outsmart rapidly dividing melanocytes. Sadly no. The venerable figure that he is, I can just about picture him telling a group of despondent young residents that it would be naive to think that a terminally ill doctor might avoid the fate of many of his patients.
Oliver Sacks dying of metastatic melanoma may have been just another story of misfortune in a world spilling over with bad news were it not for something that caught my eye towards the middle of his column. He lists symptoms of nausea, loss of appetite, chills and sweats and a pervasive tiredness, all cardinal signs of worsening cancer. He tells us he is still managing to swim although the pace is slower as he pauses to breathe. And then, he says something utterly obvious and yet, thoroughly remarkable: “I could deny it before but I know I am ill now.”
In a piece of achingly beautiful writing, this observation may bypass the typical outsider but as an oncologist, it struck me as the essence of what it takes to die well – the concession that all the well-intentioned therapy in the world can no longer prevent one from going down the irreversible trajectory of death.
This recognition allows patients to halt toxic treatment, opt for effective palliation and articulate their goals for the end of life. It permits their oncologist to open up new conversations that don’t include the latest million-dollar blockbuster therapy with a bleak survival curve but do mention the therapeutic benefit of teaming up with hospice workers to write letters, preserve photos and record memories. I would say that this candid admission from a patient is the difference between bemoaning death as a medical failure and viewing life as a welcome gift.
He had determined that there was to be no conversation about her progressive cancer or the fact that she lay dying. Her experience was unacceptable yet the impasse dreadful and ethically troubling.I found myself thinking of a former patient who came into hospital dying of liver failure from metastatic bowel cancer. Her jaundiced skin was practically glowing and she had a resulting insatiable itch. There was not a single comfortable position she could find and it soon became clear that that she needed continuous sedation for comfort. But before I sedated her I needed to be sure that she understood her terminal condition, difficult given that the liver failure was causing agitation. The problem was that her husband was permanently stationed at her bedside and would not hear of me mentioning any bad news to the patient.
One morning her husband was delayed but she needed urgent attention so I walked in alone to find a clearly distressed patient. Looking surreptitiously around the room, and temporarily alert, she whispered, “What is happening to me?”
I sat down and held her hand, noting a trail of bleeding scratch marks.
“Do you want me to tell you?”
Before she could answer, her husband roared from behind me, “How dare you plot to scare my wife like that in my absence? Get out!”
As I covered my ears against the litany of abuse, the patient’s terrorised eyes briefly rested on mine. Sorry, they seemed to say, I am really sorry. Refusing to be mollified by the palliative care staff the man virtually dragged his dying wife home. He made a mockery of her end of life care and left me with a searing memory of my failure to help a dying patient. But I also try to remember that he loved her and just couldn’t bear the thought of letting her go. Letting go is hard.
Doctors fail patients in various ways but in some ways it is easier to fail patients when they or their family deny impending death. They are the ones who deserve our greatest consideration and patience but the truth is that it’s taxing enough to treat intractable pain, omnipresent nausea or pervasive melancholy without having to take on the onerous task of saying, “Believe me, you really are dying.”
Unlike suturing or locating a pulse, dealing with death does not become easier with time. If you care about your patient, it always hurts. It hurts when you fail to cure them and it hurts when you fail to help them die. Patients who can get even part of the way to acknowledging their mortality ultimately do themselves, their relatives and even their oncologists an untold favour.
But of course, it’s one thing to understand your mortality and quite another to articulate your feelings for the world to scrutinise. At his diagnosis Oliver Sacks wrote, “I cannot pretend I am without fear. But my predominant feeling is one of gratitude.” Those insightful words brought inspiration to untold patients.
But the doctor who brought to us the man who mistook his wife for a hat isn’t about to mistake death for what it is. Now he reminds us with all the poise and dignity we have come to expect of him that there is value in embracing our mortality, that there is an art to dying, and before he goes, he might just show us how. For this and so much more, we owe him.

沒有留言:
張貼留言